Most of you have probably never heard of myeloperoxidase, but this mostly helpful enzyme has been the catalyst for one of the most widespread medical myths in the modern age: The Green Snot Myth.

For decades, the prevailing wisdom of the masses promulgated that if your mucus has turned green it means you have a bacterial infection and need antibiotics. While this is occasionally true, most green mucus is no more than the natural byproduct of your immune system with its advantageous enzymes cleaning house.
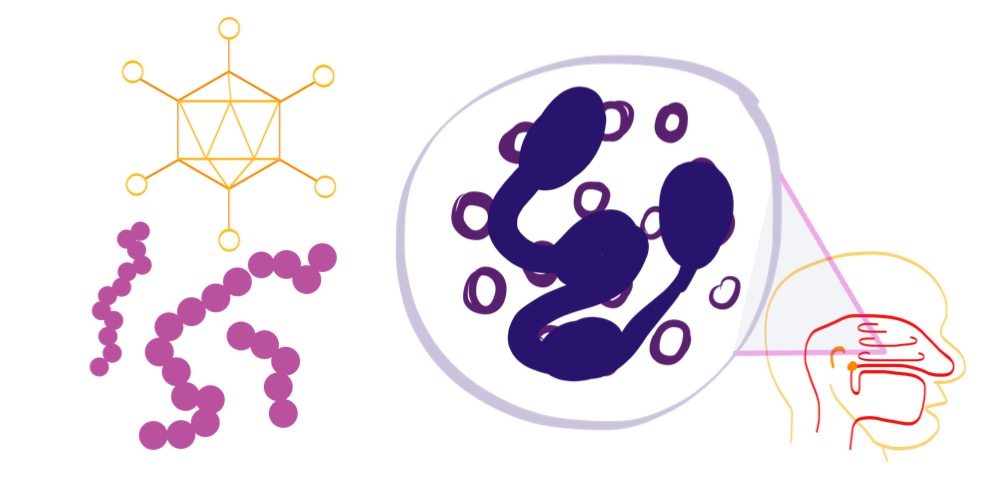
Barring several genetic disorders, we all have white blood cells floating around in our blood and tissues. These cells fight invading bacteria- and virus-infected cells and clean up debris using multiple enzymes, specialized proteins that assist chemical reactions. One type of white blood cell, the neutrophil, uses the enzyme myeloperoxidase to destroy cells affected by bacteria and viruses, and in the process oxidizes iron contained within those cells. The resulting chemical compounds reflect a greenish-yellow hue, giving our mucus a distinctive color.
Fortunately for us, those neutrophils spring into action all the time. They work to protect us from invaders throughout the day and night, even if we don’t have symptoms of illness. Unfortunately, this means that mucus sitting in the airway over time will ALL turn green. This fact makes mucus color far less important than other factors when determining bacterial versus viral infections or allergies.
Differentiating between a viral upper respiratory infection–which affects the sinuses, nasal cavities, turbinates, ears, pharynx, larynx, trachea and upper bronchi–and acute bacterial rhinosinusitis is difficult. Many symptoms that we associate with these infections represent the body’s natural response to several different invaders. Mucus production, swelling of the thin mucosa lining the nose and throat, and even fever protect against invaders of all types, from allergens to infectious disease. To help, the Infectious Diseases Society of America proposed a handful of guidelines for whether antibiotic treatment is appropriate for you or your children.
1) If symptoms have lasted longer than 10 days with no evidence of clinical improvement.
While 10 days can seem like forever with a sick child, most viral URIs can last 7-10 days. Often, the first 3-4 days are the worst, but symptoms like cough and congestion can take several more days to resolve. Most physicians recommend what we call conservative management in the early going. Treat the symptoms with simple and proven methods like oral pain relievers or anti-inflammatories. Get plenty of sleep and drink plenty of fluids, like water or oral rehydration solutions. Some studies show humidifying the air, especially when sleeping, can improve symptoms. More than anything, patience and rest are the key. Symptoms like fever and cough may make us feel bad, but they exist to protect us.
2) If symptoms are severe from day one, with not only purulent nasal discharge (which is NOT just green snot–see above), but high fever (>39°C or 102°F) and facial or tooth pain for 3-4 consecutive days.
As above, the presence of green mucus can indicate an immune system response to bacterial invasion, but the consistency is often far more important than the color. The presence of pus–a milky white material consisting of bacteria, white blood cells, and their byproducts–gives the mucus a consistency not unlike yogurt. Early changes in mucus combined with high fever and facial pressure can definitely support a diagnosis of bacterial rhinosinusitis, so seek medical attention appropriately.
3) If symptoms seem to worsen at day 5 or 6 after an initial improvement, especially with new onset of fever, headache, or the aforementioned changes in nasal discharge.
Many bacterial infections occur secondarily as a result of the physiological and chemical changes taking place during a viral infection. Swelling in the nose and throat increase the risk of bacteria getting trapped with an ample supply of energy-rich mucus for food in the sinus cavities where they don’t belong. Well-fed bacteria tend to reproduce rapidly, meaning bacterial overgrowth and infection. When the symptoms of a URI worsen suspiciously on day 5 or later, it’s time to make the trek to the physician for further evaluation.
While all of us want our sick children to feel better, we need to balance the risks and benefits. Inappropriate use of antibiotics carries significant risks–drug-resistant bacteria, the harms of killing off beneficial bacteria in our GI tract, and the potential for developing allergies to many antibiotic classes. Conversely, bacterial infections can cause significant complications and life-threatening illness. Unfortunately, our current understanding and diagnostic capability is not such that we can quickly or easily differentiate in the case of upper respiratory infection. Therefore, it falls on all of us to act responsibly and choose wisely when seeking treatment from physicians or other healthcare professionals. Sometimes, all we really need is a little tincture of time and some sleep.
Cover your coughs, wash your hands, and take time off if able. And as always, if you have any questions or concerns, you should contact your primary care physician or another qualified healthcare professional.
For more information check out FamilyDoctor.org or the original paper on IDSA Guidelines.



One point that’s alluded to but not really brought out: fever is part of our immune response and helps us get better faster, so unless it hits 40C, leave it alone. Don’t freak out and pump Tylenol/Advil into them (or yourself) at the first sign of a fever, trying to bring it down. You just prolong the illness that way.
The only caveat: newborns (up to about 3 months, IIRC) can’t maintain their body temperature as well, so fevers can get out of control quickly, and thus need to be closely monitored.
And the obligatory: I am not a doctor, and this is an opinion, not medical advice.